Physician-assisted death: Polling shows a divided membership
Deep differences exist among CMS members – including among those who are palliative medicine (PM) specialists and those with significant training in PM – on issues surrounding physician-assisted death, or PAD, though there are also areas of agreement. That’s what was revealed by a February 2016 survey of CMS members that focused on personal support/opposition to PAD, desired policy and the role for CMS in regard to efforts to legalize PAD in Colorado, concerns and priorities if a PAD law/ballot initiative passed in Colorado, and interest in enhanced end-of-life education for patients and physicians.
- Overall, 56% of CMS members are in favor of “physician-assisted suicide, where adults in Colorado could obtain and use prescriptions from their physicians for self-administered, lethal doses of medications,” (including 31% “strongly”), while 35% are opposed (including 25% “strongly”).
- Among those with at least some training in palliative medicine (42% of members overall), support stands at 56% (29% “strongly”) and opposition stands at 39% (29% “strongly”).
- Among the somewhat narrower audience of those with at least “significant” training in PM (14% of members), support stands at 52% (including 24% “strongly”) and opposition stands at 41% (with 32% “strongly”).
- Among those who “frequently” treat patients in later stages of a terminal disease, support stands at 50% (28% “strongly”) and opposition stands at 41% (32% “strongly”); among those who “sometimes” treat terminally ill patients, support is 51% (28% “strongly”) and opposition is 38% (27% “strongly”); among those who “rarely” or “never” treat such patients support is 65% (37% “strongly”) and opposition is 23% (18% “strongly”).
- Physicians in Denver are considerably more supportive (62%-24%) than those in smaller cities in Colorado (49%-41%) and those in small towns or rural areas (48%-45%).
- Those who are under 45 and those who are over 65 are most supportive (at 60% and 66%, respectively), while those 46-64 are less supportive (50%).
Priorities are clear: Protect patients, physicians
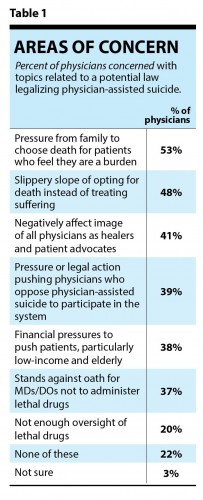
In the event that the legislature or voters enact PAD in Colorado, CMS members want to see fundamental protections included for both patients and physicians. (See table 1.)
Those taking the survey read the following: “While it is impossible to know the future, CMS needs to determine its members’ priorities should legislation or a ballot initiative pass that would legalize physician aid in dying, also known as physician-assisted suicide. Please bear in mind that these questions are in no way intended to suggest that CMS is taking a position in favor of physician-assisted suicide; our goal is to understand what members would prioritize in this hypothetical scenario.”
- One-half of CMS members (53%) are concerned that a law regarding PAD could result in pressure from family to opt for death and 48% are concerned that such a law could lead to a “slippery slope” of opting for death.
- Two-in-five (41%) are concerned about how such a law would impact the image of physicians, 39% are concerned that there could be pressure or legal actions on physicians who do not want to participate in such a system, 38% are worried about financial pressures to push low-income or elderly patients toward death and 37% are concerned because PAD goes against the oath for MDs/DOs to not administer lethal drugs.
CMS members are nearly unanimous in demanding that any such a law include key provisions to protect patients and physicians. (See table 2.)
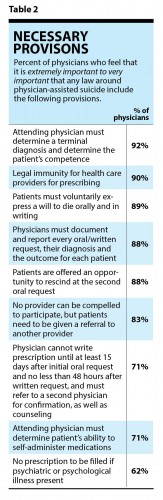
- Nearly all physicians say that having a requirement that the attending physician must determine a terminal diagnosis is “extremely” or “very” important (92%), that there should be legal immunity for health care providers (HCPs) for prescribing under the terms of the law (90%), that patients must voluntarily express a will to die (89%), that physicians must document and report at every stage (88%) and that patients should be offered a chance to rescind at the second oral request (88%).
- Almost as many physicians (83%) also feel it is important that “no provider can be compelled to participate,” but patients should receive a referral to another provider.
Opportunity: Heightened awareness of end-of-life care
Heightened awareness around end-of-life care, for patients as well as physicians, is seen as a critical step forward, whether legislation or ballot initiatives proceed or not.
- 3% of the CMS physicians in active practice in the survey report that they are a palliative medicine (PM) specialist, another 11% have received “significant” training in PM, and another 28% have had “some” training; 56% have had “none.”
- Overall, 26% of CMS members “frequently” care for patients who are “in a later stage of a terminal illness, or are in a stage of their life where they need to consider options for their final stages of life.” Another 28% say they “sometimes” care for such patients, while 22% say “rarely” and 12% say “never.” (11% say “not sure,” mostly among medical students.)
- Among physicians who say “frequently,” 30% report either being a palliative medicine specialist or having “significant” training in PM, while 41% say they have had “some” training and 28% say “no training.”
- Among those who say “sometimes,” 12% have had “significant” training, 41% have had “some” training and 54% say “no training.”
Among those who “frequently,” “sometimes” or “rarely” take care of patients in later stages of terminal illness, one-half refer to a palliative care specialist either “every time” (19%) or “most of the time” (35%), while another one-quarter do so either “sometimes” or “rarely,” and 8% do so “never” (while 15% say “not sure”).
- Among PCPs who take care of patients in later stages of terminal illness, 27% refer to a palliative medicine specialist “every time,” 50% do so “most of the time” and 19% do so “sometimes” or “rarely” (while only 3% say “never”).
The most significant barrier to greater referrals to palliative medicine or hospice care cited by physicians who care for patients in later stages of terminal illness is patient reticence to discuss these issues (with 27% among all CMS members, and 47% among those who “frequently” care for such patients). (See table 3.)
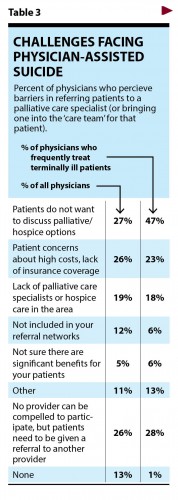
- Other barriers include high costs, insurance coverage (26%) and lack of PM specialists in their area (19%).
- Notably, concern about access to PM specialists or hospice care being available for patients locally scored much higher among members from towns/rural areas.
- Three-quarters (76%) say it is either “extremely” (45%) or “very” (31%) important that CMS “explore programs (webinars, trainings, connection to expert resources in Colorado, connection to peers in Colorado) focused on helping providers better address end-of-life care issues with their patients,” while 18% say this is “somewhat” important and 3% say it is “not very” or “not at all” important.
- A somewhat greater percentage (81%) say it is either “extremely” (52%) or “very” (29%) important that CMS “encourage a stronger focus among health care providers in Colorado around public education on end-of-life issues,” while 14% say this is “somewhat” important and 2% say “not very” or “not at all.”
Conclusions
Members want to see CMS promote better education of the public and physicians around end-of-life care. Increased awareness among the public of the options that are available, including palliative medicine and hospice care, would be very welcome. Efforts to ease discomfort for patients and their families around discussing these issues can help Colorado’s physicians care for the vast majority of patients who will not seek PAD, so they can die with dignity with the support and care of a trusted physician at their side.
Methodology
This survey was administered online by the Colorado Medical Society. The survey was in the field from Feb. 2-16, 2016. A total of 618 Colorado Medical Society members (including medical students and physicians) responded to the survey, for a margin of error of +3.9% at the 95% confidence level. A series of three focus groups was held to inform the development of the survey questions, including a group each with supporters, opponents and those “in the middle” regarding PAD.
A note on terminology
Given what we learned in the focus groups, the survey was introduced as being about “physician-assisted suicide, also referred to as physician aid in dying and physician-assisted death.” After much deliberation, we chose these terms (as opposed to “Death with Dignity” or others) because physicians who oppose PAD noted that phrases like “Death with Dignity” do not recognize the fact that physicians already help patients die with dignity via current practices (such as palliative sedation or voluntary withdrawal of food/water). We felt this was the least biasing language, and proceeded accordingly.
Posted in: Colorado Medicine

Comments
Please sign in to view or post comments.