Cover: DOJ challenges mergers
Colorado Attorney General joins suit
by Kate Alfano, CMS Communications Coordinator
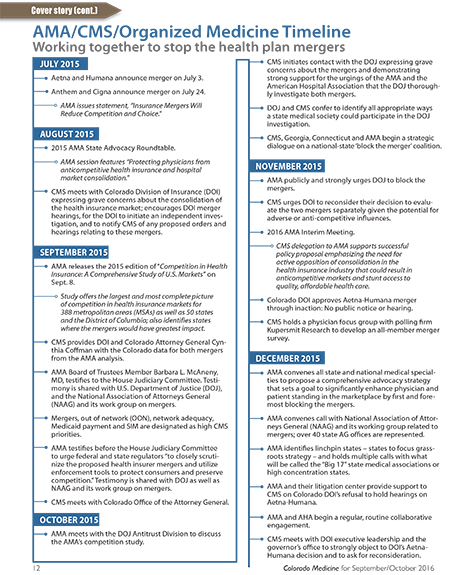
In late July the Department of Justice (DOJ) filed suit in the U.S. District Court for the District of Columbia challenging the proposed mega-mergers between Anthem-Cigna and Aetna-Humana, the culmination of more than a year of methodical research and close collaboration with antitrust experts from the American Medical Association (AMA), the Colorado Medical Society and 16 other state medical associations who worked together and with their physician members to develop a compelling economic and legal case for competition.
The DOJ’s extraordinary effort is the first comprehensive legal challenge in many years to the attempts of the nations’ largest and most influential health plans to consolidate their market share and directly and indirectly influence the physicians who provide care in those communities.
When the mergers were announced in July of last year, the AMA and state medical societies responded swiftly with a campaign detailing how the mergers would increase health insurance market concentration and reduce competition. The aim was to demonstrate that the proposed mergers would have negative long-term consequences for health care access, quality and affordability in states across the nation. This response would prove to be a case study in how combining the first-person stories from practicing physicians and the strength of medical organizations – with the data, expertise and experience of the AMA team – can fuel the federal government’s oversight of these anticompetitive power-plays.
In September 2015, the AMA released an in-depth analysis of the mergers’ potential impact on markets and access to care, sharing the results with the DOJ, states and the general public. The findings were clear, staggering and authoritative: The combined impact of the proposed mergers would exceed federal antitrust guidelines designed to preserve competition in as many as 97 metropolitan areas within 17 states, including Colorado. And the findings perfectly matched the DOJ’s definition of enhanced market power: “A merger enhances market power if it is likely to encourage one or more firms to raise price, reduce output, diminish innovation, or otherwise harm customers as a result of diminished competitive constraints or incentives.”
The AMA also highlighted research published in a leading academic journal establishing that the 2008 United HealthGroup Inc. merger with Sierra Health Services in Nevada resulted in higher premiums. This fact-based evidence disproved the insurers’ central claim that savings would be passed on to consumers. Both the broader competition survey and the Nevada study earned prominent media coverage and frequent citation in testimony before Congress and in the states.
In December 2015, the AMA identified the 17 states where the mergers would have the most harmful impact on patient care delivery and formed a coalition with their state medical associations to block the mergers. The AMA worked closely with CMS in piloting a physician survey relating to the monopsony issues raised by the proposed mergers that was sent to physicians in many of the 17 states. The survey covered not only the likely direct deleterious effects of the mergers on patients in the form of higher premiums and poorer plan quality, but also the likely indirect adverse effects on the quality and quantity of physician services caused by health insurer “buyer” or “monopsony” power in contracting with physicians.
The survey responses were powerful, alarming and persuasive to the DOJ investigators, who methodically interviewed numerous physicians in many of the concentrated states identified by the state medical advocates as having extensive experience negotiating plan contracts.
In Colorado, a majority of CMS members (68 percent) opposed allowing the mergers to proceed, including 48 percent who “strongly” opposed it. Among physicians in active practice, 73 percent said they oppose (54 percent “strongly”). Among decision-makers – physicians who participate directly in contract negotiations with commercial insurers – opposition stood at 79 percent (63 percent “strongly”). And nearly all decision-makers (who make up one-third of CMS members, and are largely concentrated among office-based, smaller specialty care practices) expressed a belief that contract negotiations will be less favorable to physicians if the mergers are approved, with 85 percent saying as much.
Data from the AMA and federal Centers for Medicare and Medicaid Services showed that the Aetna-Humana merger would likely enhance market power or potentially raise significant competitive concerns in five Colorado counties: Boulder, Mesa, Larimer, Pueblo and Weld. The market analysis served as a strong foundation for CMS and the component societies in these markets to make the case to the DOJ, state regulators, and lawmakers to carefully scrutinize and block the mergers.
In the face of this compelling information, the plans threw every conceivable legal theory into their case, spending millions of dollars on legal, banking and advocacy services. When Anthem argued that consumers will benefit by its reduced costs in paying for physician services – suggesting the Affordable Care Act’s Medical Loss Ratio (MLR) will prevent the insurers from pocketing excess profits – the AMA secured a letter from Washington and Lee law professor Tim Jost, the author of the ACA’s MLR regulations. His letter, which was addressed to the Florida attorney general and shared with the DOJ before it filed its merger challenges, explained that MLR is no substitute for competitive health insurance markets and does not – nor was it intended to – prevent health insurers from exercising market power.
And when Aetna and Humana argued that the new entity’s massive Medicare Advantage share would be of no consequence because Aetna must compete with the U.S. government and its traditional Medicare offering, the AMA secured a letter from 20 prominent health economists (including former FTC Bureau of Economics Director Marty Gaynor) outlining why they are not the same market. Again, this letter was delivered to the DOJ and state attorneys general. Consequently, the DOJ’s complaint against Aetna-Humana reflects these AMA efforts; a section of their complaint is devoted to Medicare Advantage as a relevant product market and covers the points outlined in the economists’ sign-on letter.
As a direct result of these comprehensive efforts, Missouri’s insurance department found that Medicare Advantage does not compete with traditional Medicare and refused to approve the Aetna-Humana merger. The California Insurance Department acted soon thereafter, extensively referencing the AMA’s concerns as a basis for its powerful opposition to the mergers on both monopoly and monopsony grounds. The DOJ and a number of states ultimately decided to challenge both mergers. Among the 18 states and the District of Columbia that joined one or both of the lawsuits, 12 were among the 17 states in the AMA coalition.
A merger of this magnitude would compromise physicians’ ability to advocate for their patients; in practice, market power allows insurers to exert control over clinical decisions, which undermines physicians’ relationships with patients and eliminates crucial safeguards of patient care.
The DOJ lawsuit is not the end of the story; both companies have stated that they plan to vigorously defend it. What will be required for the long haul is a steadfast link between the AMA and the state medical societies, as well as thousands of grassroots physicians, to ensure health care markets can continue to function as intended, where the business relationships between plans and medical practices are balanced and competition is over the value of services, not market share.
Posted in: Colorado Medicine | Cover Story | Practice Evolution | Payment Reform | Interacting With Payers | Initiatives | AMA

Comments
Please sign in to view or post comments.