All-member opioid survey
Your voice: Physician collaboration, CMS advocacy needed to address the crisis
by Benjamin Kupersmit, President, Kupersmit Research
Editor’s note: The Colorado Medical Society has been deeply involved in reversing the public health crisis caused by opioid abuse and misuse for the past five years. Colorado physicians and other health care providers have been nationally recognized by the American Medical Association for using the Colorado state prescription drug monitoring program (PDMP) more than 1.5 million times in 2016 (a 122-percent increase from 2014), and for decreasing overall opioid prescriptions by nearly half a million since 2013.
Working with Gov. Hickenlooper’s Colorado Consortium for Prescription Drug Abuse Prevention and many other stakeholders to end harm from opioid-related abuse and misuse, CMS and other physician-led organizations such as COPIC, the CU School of Medicine, the Colorado Permanente Medical Group, and CPEP, among others, have led the charge to educate physicians to change their prescribing practices and their approach to pain treatment to combat the crisis. As part of that effort, CMS recently surveyed its members on:
- Current perceptions of the prescription drug abuse crisis,
- Participation in efforts (including PDMP and continuing medical education) to mitigate the crisis, and
- Reactions to proposals from the governor’s office to further address the crisis.
The results show a deep awareness of the opioid crisis, and that physicians are actively working to combat the problem.
CMS Committee on Prescription Abuse Chair, John Hughes, MD, reviewed the results and said, “I would have been extremely disappointed had this survey outcome not shown progress after all the work that CMS and other physician-led organizations have put into reversing the opioid crisis in our state. These numbers demonstrate that the combined efforts of CMS, COPIC, the CU School of Medicine, and the Colorado Consortium are working for Colorado.”
CMS contracts with Kupersmit Research to conduct CMS surveys. The firm certified the opioid crisis survey for accuracy with a margin of error of +3.8% at the 95% confidence level. What follows is their official survey memo.
Kupersmit Research is pleased to present the results of the 2017 CMS member survey focusing on the prescription drug abuse crisis in Colorado. Nearly 700 CMS physicians completed the survey questionnaire.

Landscape
- A majority of CMS physicians agree that prescription drug abuse is “a very serious problem, among the top public health issues we face” (with 58%), while another 6% feel it is “a full-blown crisis, the No. 1 public health crisis we face.”
- Another 32% say it is “a serious problem, but not the top problem we face in public health.”
- Prescription drug abuse is seen as a patient management issue, with 62% saying it is a problem of “patient education and management,” versus 3% a “law enforcement problem” (33% say “both equally”).
- CMS physicians are most concerned with the “misuse, abuse and diversion” aspect of the prescription drug abuse crisis.
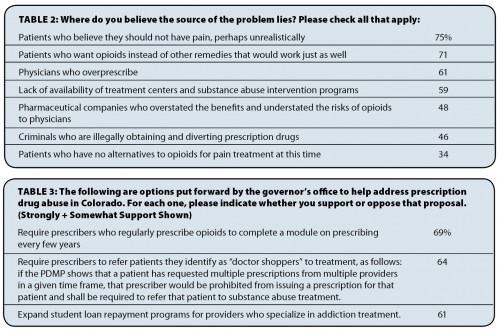
Roots of the problem
- CMS physicians are most likely to believe the root of the prescription drug crisis lies in patient expectations around pain and opioids, followed by “physicians who overprescribe” and a lack of treatment centers and intervention programs.
- Comments suggest a complex set of factors contributing to the perception among physicians that their colleagues overprescribe:
“Ongoing overprescribing of opioids for chronic musculoskeletal pain, wisdom teeth extraction, headaches, abdominal pain, post-surgical pain for more than a few days, etc. Ongoing underfunding of treatments that actually help such as lifestyle modification (exercise, diet and relaxation skills training), cognitive and behavioral therapy, and minimally invasive treatments such as acupuncture, non-steroidal trigger point injections, manual therapy, etc.”
- Physicians repeatedly point to patient satisfaction surveys and the designation of pain as the “fifth vital sign” (and the leverage patients feel they have over physicians as a result) as key factors contributing to the crisis as well:
“Patient satisfaction scores that overemphasize patients being happy with their treatment of pain.”
“Joint Commission recommendations years ago that needed to treat pain as the fifth vital sign and that no patient should ever have pain.”
“I have been reported to medical board for not treating patients’ pain. Hard to win when we get in trouble for over-prescribing from one entity and from patients reporting us to medical board.”
Taking Action: Checking the PDMP, taking CME
- Overall, 46% of CMS physicians report that they use the PDMP “all the time” or “pretty often” (up from 27% in 2013 CMS survey research).
- Use of the PDMP is considerably higher in key specialties: family medicine (91%), emergency department (87%) and internal medicine (83%).
- Comments suggest that lower usage rates among some surgeons may be because they believe short-term prescriptions for acute pain are not as relevant to the opioid crisis.
“Haven’t used the program (PDMP). I only treat post-operative short-term pain with opioids.”
“My patient are post-surgical and only receive short-term narcotics if needed. I only check the registry if a patient is making unreasonable requests for additional prescriptions beyond one to two weeks, which is rare.”
- Nearly three-quarters (70%) of CMS physicians report taking CME regarding opioids in at least the past two to three years.
- Physicians in internal medicine (88%), family medicine (84%) and the emergency department (83%) are more likely to say they have had CME in the past two to three years.
Next Steps: Support proposals, but concerned resources are inadequate
- As Table 3 shows, a solid majority of physicians support a range of potential proposals to help mitigate the prescription drug crisis.
- Just under two-thirds support efforts to better identify “doctor shoppers” through the PDMP and then refer these patients to treatment, as well as expanding student loans for those who specialize in addiction treatment.
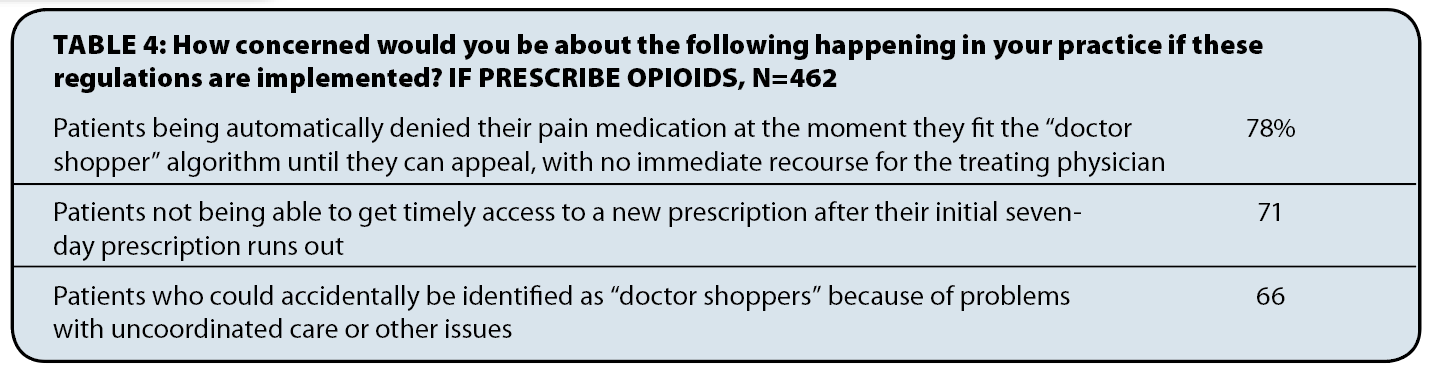
- At the same time, there is significant concern about these proposals if adequate safeguards are not in place for patients who are identified erroneously as “doctor shoppers” or for patients who are unable to get needed medication because of other potential problems that might arise.
- Furthermore, just half (46%) of those who prescribe opioids (n=462) currently know where to refer someone for substance abuse treatment, while 42% do not (and 12% are unsure how to respond).
- Fully 83% of those who currently prescribe opioids are “not confident” that Medicaid patients will have access to a substance abuse specialist who accepts Medicaid.
- Two-thirds (66%) are “not confident” that private insurance patients will have in-network access to a specialist for substance abuse treatment.
Conclusions
CMS physicians express a clear understanding that prescription drug abuse is a very serious public health issue, but we do not see a level of urgency reflective of “the most serious public health crisis in 125 years,” as the Colorado governor’s office has stated. At the same time, physicians understand that responsibility for addressing the problem is theirs; virtually no one believes this is a problem for only law enforcement to address.
Prescription drug abuse is viewed as a complex problem with multiple root causes and myriad harmful impacts, and we hesitate to simplify the hundreds of individual statements of concern or anger or anxiety expressed in the survey’s open-ended replies. The overarching trends from the physician perspective, we believe, are perhaps twofold:
- First, societal expectations regarding pain – bolstered with the inclusion of pain as the “fifth vital sign” in policy, along with the usage of pain as a metric in physician satisfaction surveys – are generating demand, and patients have leverage (e.g., reporting physicians who refuse to prescribe opioids to administration or the medical board), to push physicians to prescribe.
- Second, a majority of CMS physicians feel that their colleagues are over-prescribing, with significant disagreement between specialties, and tremendous levels of stress and anxiety in specialties viewed as over-prescribers by others.
CMS physicians are already working and taking steps to mitigate the crisis, such as checking the PDMP (for which usage has jumped substantially since 2013) and taking continuing medical education on opioids. The survey suggests that physicians are somewhat split on increasing these requirements, and would perhaps need to see clear evidence that such increased requirements will make a difference moving forward.
We do see significant support for efforts to better identify doctor shoppers and limit their access to opioids and refer them to substance abuse treatment. However, there is significant concern that patients with private insurance and Medicaid will not have affordable access to substance abuse treatment, and many physicians are currently unaware of where they would refer such patients. There is also significant concern in the survey about the lack of access to alternative treatments to opioids.
In our view, the survey suggests a range of opportunities for CMS and its member physicians to pursue:
- Educate patients through direct physician-to-patient education (pamphlets, conversations), ideally bolstered with messaging and advertising aimed at the wider public.
- Convene physician leaders across specialties, perhaps starting with those most affected by the crisis.
- Reach out to hospital administrators to let them know that physicians have significant concerns about including pain in satisfaction surveys and other key performance indicators.
- Join national efforts to address issues with private and public payers around access to alternative treatments to opioids, as well as substance abuse treatment; efforts to remove the use of pain as the “fifth vital sign” should be joined by CMS as well.
- Integrate PDMP checks into daily practice habits and EMR (particularly for surgeons who might feel that short-term prescriptions are not as relevant to the crisis).
Methodology
This survey was administered online by the Colorado Medical Society. 673 members gave a full response to the survey, of a total of 5,815 CMS members emailed (with 743 beginning the survey), giving a 12% response rate. The survey was conducted Sept. 6-25, 2017; for the sample of 673 members, the margin of error is +3.8% at the 95% confidence level.
Posted in: Colorado Medicine

Comments
Please sign in to view or post comments.