2017 all-member survey
Members express clear desire to overhaul health care delivery system in Colorado
by Benjamin Kupersmit, President, Kupersmit Research
Kupersmit Research is pleased to present the results of the 2017 CMS member survey focused on member priorities for reforms to the health care delivery system in Colorado.
(Unless otherwise indicated, data below is among physicians in active practice who accept commercial insurance (n=488, approximately 80 percent of CMS members overall). We also focus on “decision-makers” in their practice who participate in contract negotiations with payers, (typically owners/partners in office-based practices; n=113, approximately 20 percent of CMS members).
CMS physicians in active practice who contract with insurance, and particularly decision-makers, express significant frustration with commercial payers and a clear desire for reform:
- Physicians, and particularly decision-makers, feel they must contract with commercial payers to remain financially viable, with 79 percent of decision-makers saying as such regarding top Colorado insurers United HealthCare and Anthem.
- Yet, just 28 percent of decision-makers say criteria for participation have been explained at least “somewhat” clearly; among the 30 percent of decision-makers removed from a network or plan in the past year, just one-third (34 percent) were given written notice and just 9 percent say they were given an explanation for their removal.
- Nearly three-quarters of CMS active practice physicians (70 percent) say that their patients’ medications are changed by their insurer; a 2015 member survey found that 66 percent feel medication regimen changes by insurers have caused adverse events for their patients.
- A majority (54 percent) of active practice physicians and 79 percent of decision-makers say patients have discontinued care because of insurance changes.
- Nearly half (46 percent) of active practice physicians and 63 percent of decision-makers say they have difficulty finding in-network referrals.
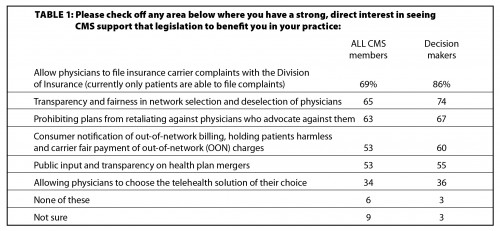
- We see significant support for key legislative reforms at the state level among those surveyed:
- Sixty-nine percent of all active practice CMS physicians and 86 percent of decision-makers say efforts to allow physicians to file with the DOI would “directly benefit” them now.
- We see similarly strong scores for addressing network selection and deselection (65 percent among all, 74 percent among decision-makers) and protection of physicians from retaliation by health plans (63 percent among all, 67 percent among decision-makers).
- Other priorities include addressing OON billing issues (with 53 percent among all and 60 percent among decision-makers) and ensuring public input and transparency for health plan mergers (with 53 percent among all and 55 percent among decision-makers).
Physicians want local solutions now
Over the years, we have watched as more and more physicians move to an employee role. This survey reminds us that the choice to be employed versus an owner/partner in a physician-controlled practice is being driven in some part by the desire to avoid the hassles and stress of contracting, authorizing and being reimbursed fairly and transparently by commercial insurers.
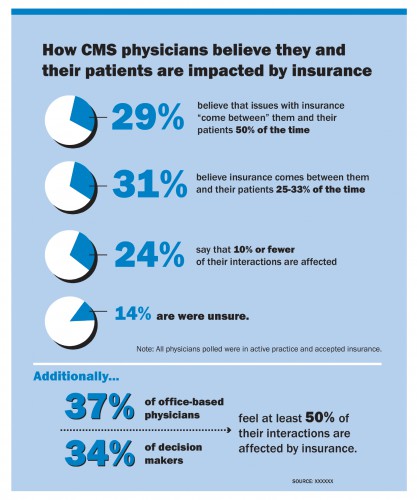
Physicians across the system report that insurance companies are interfering in medical decisions, and that lack of communication and constant change regarding insurance status are causing problems for patients and physicians alike. Not surprisingly, physicians feel that patients blame them, and that the physician-patient relationship is deteriorating from this ongoing intrusion of financial and administrative hassles into the exam room.
CMS physicians strongly believe that key reforms are needed at the state level, and expect those reforms to directly and immediately impact their practice in a positive way. Their priorities are allowing physicians to file complaints with the DOI, transparency in selection and deselection of physicians for networks, and protection of physicians from retaliation by health plans. There is also strong interest in seeing steps to address the issue of OON billing, as well as ensuring public input and transparency regarding health insurance potential mergers.
Methodology
This survey was administered online by the Colorado Medical Society. A total of 661 CMS members completed the survey, resulting in a margin of error of +3.8 percent at the 95 percent confidence level. The sample of active physicians who accept insurance (i.e., excluding med students, retired physicians, and the 1 percent in concierge practices) carries an n=488, with a margin of error of +4.4 percent, and the sample of decision-makers has an n=113 and carries a margin of error of +9.2 percent. The survey was conducted from March 1-21, 2017.
Posted in: Colorado Medicine | Health System Reform

Comments
Please sign in to view or post comments.